What to look for in your Medical Billing Reports, to understand the recurringly high Account Receivable (AR) Rate?
A high AR rate depicts negative Medical Billing performance. It is one of the main KPI that Medical Practices work on improving, to get an efficient Claim Management Process.
AR reports are used to monitor and correct a Medical Practice’s AR rate. These reports generally focus on aging buckets either by payer or by CPT codes, however if you look closing there are other important factors that should be analyzed in an ideal AR report. These factors, as discussed below, shed light on hidden aspects of your Medical Billing performance affecting your AR Rate. If your AR reports do not include the following, then your AR analysis will likely be flawed.
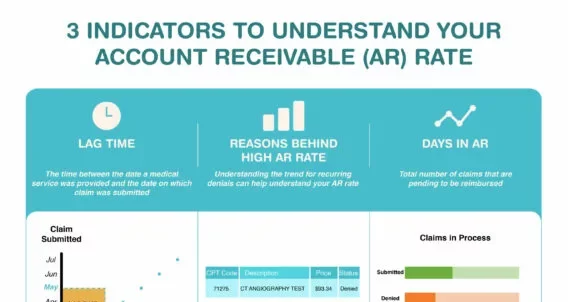
Here are 3 areas that should be analyzed in an AR report to better understand the reasons behind a high AR rate,
Lag time
- Delayed Claim Submission
- Patient Statement Lag time
Reason behind a high AR rate
- Claim in Process
- Denied Claims
- Appeals
- Incomplete Claim Data (Claims not submitted due to missing information)
- Pending patient AR
Days in AR
3 indicators to understand your Account Receivable (AR) Rate
Lag time
Lag time simply means the time/days between the date a medical service was provided and the date on which claim was submitted.
Delayed Claim Submissions
If there is an increase in lag time between the date of service and the date of claim submission then AR rate is negatively impacted. Billers usually report on the day of submission w.r.t the reimbursement received however promptly tracking the date of service can show a clear picture. This clarity will help calculate the AR rate hence improving it.
Patient Claim Lag time
If patient statements are created but not submitted then this too negatively impacts the AR rate. The date of service versus the date of submission leads to larger lag time for the claim submission, resulting in increase in AR days.
Reasons behind a high AR rate
Denial Rate
Read our blog for more information on denials
Tracking the number of denied claims as well as understanding the trend for recurring denials can help understand your AR rate.
A good practice to prevent recurring denials, is to analyze the list of CPT codes for the claims that are denied. Often it happens that billers submit the same CPT codes without rectifying the issue. Identifying the errors can help prevent recurring denials for the same CPT code saving time and improving the AR rate.
Appeals
Tracking the number of claims that are resubmitted after corrections, is necessary to understand the reasons for a high AR rate.
Mostly, AR rate is tracked back to denied claims while appealed claims are left out of the picture. This presents an incomplete and unclear report. A good practice is to track the number of claims in denials as well as appealed claims to better understand the AR rate.
Incomplete Claim Data (Claims not submitted due to missing information)
Often claims are put aside due to missing or incomplete information. These claims are pending to be submitted, until the information on them is completed. These lead to increase in account receivable days because the service was rendered but the reimbursement is not received.
Claim in Process
Claims that are submitted and are under process are often left out while calculating the AR rate. This effects the authenticity of the AR report. Hidden/missing information results in incorrect AR calculations, negatively effecting the improvement strategies for AR rate.
Pending Patient AR
Payments pending from patients’ side also result in a high AR rate. It should be added in the AR report to show the real picture and to enable Medical Practitioners understand the reasons for pending reimbursements.
Days in AR
Usually reports show an average on total number of claims that are pending to be reimbursed. A better practice is to break down these claims depending on their payer e.g., if Medicare claims are pending reimbursements than rectifying the under-laying cause for this specific payer can help prevent such delays in future, hence positively impacting the overall AR rate.
Attached is an infographic that simplifies the above-mentioned points and will help you understand your AR rate.
AltuMED is a Medical Billing Service and Solution Company that understands the importance of prompt, systematic Medical Billing Performance Analysis. Why not contact us for a complimentary analysis that can help us understand the reason for increase in your AR rate?
Subscribe to Our Newsletter!
Subscribe to Our Newsletter!
Enter Your Email Address. We Promise We Won't Spam You
Relevant Articles
Categories
Informational
Educational
Medical Billing Software