
Highly Anticipated 2024 Coding and Payment Policy Changes (E/M Edition)
We have got some significant changes for you to go through for the upcoming year. In this article, we’ll discuss the key important highlights of this release coming in 2024!!
Let’s begin the new year with up-to-date information that can help benefit you as a medical billing or coding firm elevate your practice management skills and make your revenue cycle improved.!
The annual update to the CPT code set created 349 editorial changes, including 230 additions, 49 deletions, and 70 revisions. With 11,163 codes that describe the medical procedures and services available to patients, the CPT code set continues to grow and evolve with the rapid pace of innovation in medical science and health technology.
The 2024 version will also be the first to offer Spanish language descriptors for medical procedures and services.
"Providing approximately 41 million Spanish-speaking individuals in the United States with an easy-to-understand description of medical procedures and services can help build a more inclusive health care environment, where language is no longer a barrier and patients can actively engage in their care,"
Lori Prestesater, AMA senior vice president of health solutions said in the release.
Let’s Begin with Changes in E/M Coding
Revisions will be made within several subsections of the evaluation and management (E/M) section to standardize the rest of the E/M sections of the CPT code set to decrease providers' administrative burden of documentation as outlined in Medicare's 2023 Final Rule. In addition, a new E/M subsection with new guidelines for split or shared services will be created. The new codes will be structured to align with the current E/M office or other outpatient services code structure.
The following updates will include:
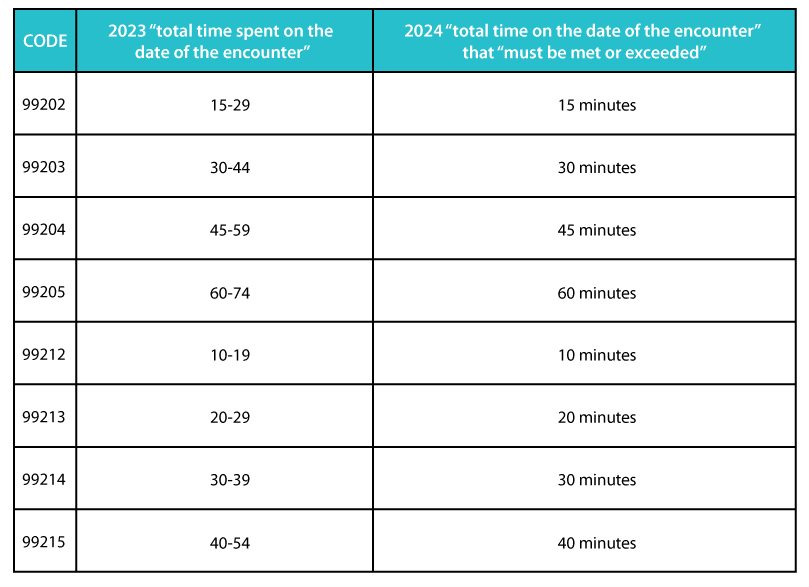
- Time ranges will be removed from the office or other outpatient visit codes for codes 99202- 99205 and 99212-99215 to align with the format of other E/M codes.
- The portion of physician’s services that may be reported for split (or shared) visits will be defined.
- Reporting instructions will be added for codes 99234-99236 [(hospital inpatient or observation care services) (including admission and discharge services)] when the duration of the visit crosses two calendar dates.
Revised Codes
The following E/M codes will be revised in the CPT 2024 code set:
- 99202: Office or other outpatient visits for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision-making. When using time for code selection, 15-29 minutes of total time is spent on the date of the encounter.
- 99203: Office or other outpatient visits for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and a low level of medical decision-making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.
- 99204: Office or other outpatient visits for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and a moderate level of medical decision-making. When using time for code selection, 45-59 minutes of total time is spent on the date of the encounter.
- 99205: Office or outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and a high level of medical decision-making. When using time for code selection, 60-74 minutes of total time is spent on the date of the encounter.
- 99212: Office or another outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and straightforward medical decision-making. When using time for code selection, 10-19 minutes of total time is spent on the date of the encounter.
- 99213: Office or another outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and a low level of medical decision-making. When using time for code selection, 20-29 minutes of total time is spent on the date of the encounter.
- 99214: Office or another outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and a moderate level of medical decision-making. When using time for code selection, 30-39 minutes of total time is spent on the date of the encounter.
- 99215: Office or another outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and a high level of medical decision-making. When using time for code selection, 40-54 minutes of total time is spent on the date of the encounter.
Nursing Facility Changes and Revisions
- 99306: Initial nursing facility care, per day, for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and a high level of medical decision-making. When using total time on the date of the encounter for code selection, 45 minutes must be met or exceeded.
- 99308: Subsequent nursing facility care, per day, for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and a low level of medical decision-making. When using total time on the date of the encounter for code selection, 15 minutes must be met or exceeded.
Changes in ‘Split/Shared’ Services E/M Visits
A notable change has been implanted for Shared E/M between multiple Clinicians managing a patient at a time. In CY 2022 carried to 2023 the policy had some flexibilities and Clinicians had options to choose from (history and physical exam, MDM, or Time). For 2024 onwards the split/shared services billing options would be retained to 'Time' spend only, (more than half of the total time spent) to set as who provided the substantive portion of the split/shared service.
Code descriptor revisions are about time.
Clarifications sought by the Centers for Medicare and Medicaid Services also prompted the CPT Editorial Panel to add revisions to the CPT 2024 code set that clarifies the reporting of evaluation and management (E/M) services. The revisions include:
- Removal of time ranges from office or other outpatient visit codes (99202-99205, 99212-99215) and aligned the format with other E/M codes.
- A definition to determine the “substantive portion” of a split/shared E/M visit in which a physician and a non-physician practitioner work jointly to furnish all the work related to the visit.
- Instructions for reporting hospital inpatient or observation care services and admission and discharge services for the use of codes 99234-99236 when the patient stay crosses two calendar dates.
- In response to requests from the Centers for Medicare and Medicaid Services, some evaluation and management (E/M) reporting codes have been revised for greater clarification.
Revision in Nursing Facility E/M Visits
For Nursing Facility Visits, a 5-minute addition has been made as a revision as clear in the descriptions below:
- 99306: Initial nursing facility care, per day, for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and a high level of medical decision making. When using total time on the date of the encounter for code selection, 45 minutes (Now – 50 minutes) must be met or exceeded.
- 99308: Subsequent nursing facility care, per day, for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and a low level of medical decision-making. When using total time on the date of the encounter for code selection, 15 minutes (Now – 20 minutes) must be met or exceeded.
G2211 implementation in 2024
G2211 Visit complexity is inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient's single, serious condition or a complex condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established).
G2211 is purposed to have the most interesting development
This add-on code will better recognize the resource costs associated with evaluation and management visits for primary care and longitudinal care. Generally, it will be applicable for outpatient and office visits as an additional payment, recognizing the inherent costs involved when clinicians are the continuing focal point for all needed services or are part of ongoing care related to a patient's single, serious condition or a complex condition.
- G2211 (definition above) is an add-on code to the office and other outpatient services, 99202–99215.
- CMS believes it will be used by primary care and other specialties who treat a single, serious condition or a complex condition with consistency and continuity over a long period. CMS is proposing not to pay for the add-on code when used with modifier 25, on the date of a minor procedure.
- G2211 can be used for the treatment of acute conditions by a practitioner who provides ongoing, care. CMS is emphasizing the relationship between the patient and the practitioner. Acute visits may not be part of continuous care, which defines G2211.
- There is no documentation or specialty associated with this code, and neither the amount to be billed is clear as of now. However, the experts estimate it to be around $20.
- All the key questions will likely be answered as CMS implements it in 2024 bringing forth all requirements and guidelines and fixing a price for it.
The new codes will align with the current E/M office or other outpatient services code structure (ie, using time or medical decision-making [MDM]) with separate codes for new and established patient encounters and the addition of a virtual check-in code that could be used to determine whether a patient needs a face-to-face visit.
Telemedicine Office Visits
CMS is finalizing that, beginning in CY 2024, telehealth services furnished to people in their homes will be paid at the non-facility PFS rate to protect access to mental health and other telehealth services by aligning with telehealth-related flexibilities that were extended via the CAA, 2023.
A CPT/RUC Telemedicine Office Workgroup was created to assess and develop appropriate coding guidance for E/M telemedicine office visits performed via audio-visual and audio-only mechanisms. The workgroup determined that a new E/M subsection with new guidelines for telemedicine services will be established in the CPT 2024 code set.
Place of Service Codes for Medicare Telehealth Services. Beginning CY 2024, claims billed with place of service (POS) 10 (Telehealth Provided in Patient's Home) will be paid at the non-facility physician fee schedule rate. Claims billed with POS 2 (Telehealth Provided Other than in Patient's Home) will continue to be paid at the PFS facility rate for non-home originating sites, such as physician's offices and hospitals.
Deleted Codes
The codes below will be deleted from the CPT 2024 code set:
- 99441: Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion.
- 99442: Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 11-20 minutes of medical discussion.
- 99443: Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 21-30 minutes of medical discussion.
- 99459: Female pelvic exam (list separately in addition to code for primary procedure)
Billed with Office Visits or as a Preventive Care service. Could not be billed separately earlier
99459 is a practice expense–only code that captures the direct practice expenses associated with performing a female pelvic exam in the non-facility Office setting during a preventive medicine service (99381-99397) or E/M service (99202-99215). As an add-on code, it should be reported only for the same date of service with the codes listed above.
Changes in Calendar Year (CY) 2024 Medicare Physician Fee Schedule Final Rule
On November 2, 2023, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that announces finalized policy changes for Medicare payments under the Physician Fee Schedule (PFS), and other Medicare Part B issues, effective on or after January 1, 2024. The calendar year (CY) 2024 PFS final rule is one of several final rules that reflect a broader Administration-wide strategy to create a more equitable healthcare system that results in better access to care, quality, affordability, and innovation.
CY 2024 PFS Rate Setting and Conversion Factor, In summary
By factors specified in law, overall payment rates under the PFS will be reduced by 1.25% in CY 2024 compared to CY 2023. CMS is also finalizing significant increases in payment for primary care and other kinds of direct patient care.
The final CY 2024 PFS conversion factor is $32.74, a decrease of $1.15 (or 3.4%) from the current CY 2023 conversion factor of $33.89.
- The Centers for Medicare & Medicaid Services (CMS) released the final calendar year (CY) 2024 Physician Fee Schedule (PFS) on Nov. 2, 2023.
- Physicians and other clinicians face significant cuts of more than 3.37 percent for CY 2024, a slightly larger cut than was outlined in the proposed rule.
- The rule, which finalizes policies for Medicare payments under the PFS and other Medicare Part B issues, will take effect on Jan. 1, 2024.
- Physicians and other clinicians face significant cuts of more than 3.37 percent for CY 2024, a slightly larger cut than was outlined in the proposed rule. Unfortunately, these cuts coincide with the ongoing growth in the cost to practice medicine as CMS projects the increase in the Medicare Economic Index (MEI) for 2024 will be 4.6 percent.
AltuMED is a Medical Billing Services and Solutions company, with more than 13 years of expertise in the industry. Our coding experts are well-versed and leave no room for error. Partner with us to avoid any coding inaccuracies.
Subscribe to Our Newsletter!
Subscribe to Our Newsletter!
Enter Your Email Address. We Promise We Won't Spam You
