What should a Medical Practice know about Obesity Counselling & MNT Billing?
Obesity is often labelled as an on-going epidemic, which has not only affected adults but growing children as well. Rising cases of obesity consequentially give birth to all sorts of detrimental diseases and conditions ranging from depression to diabetes and cardiovascular issues. The state of affairs has been worsened with prevalence of COVID.
Needless to say, a healthcare provider tries best to take notice and manage the current and associated conditions of their obese patients by different routes of therapies and counselling sessions. It is even more integral for an internist or a family physician who sees these kinds of cases on regular basis.
In this article we try to give spot-light to these seemingly simple services that can improve the overall health of the obese and over-weight patients; which a coder should be aware of and a healthcare provider shouldn’t miss.
Where the term ‘over-weight’ or ‘obese’ is used?
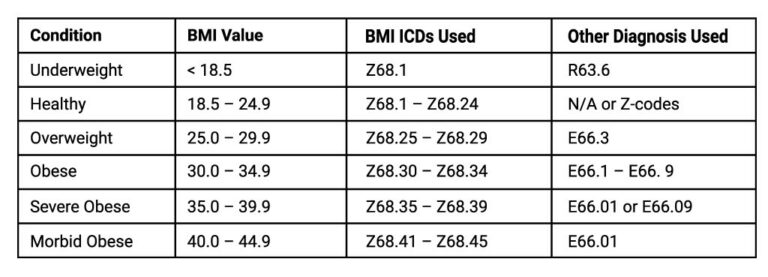
Even if these terms feel similar, they are considered quite different clinically and from a coding perspective. A patient is supposed ‘over-weight’ or ‘obese’ on the basis of their BMI (Body mass Index). We won’t go into its mathematics and calculations but as a coder you should at least know higher BMI values leans more towards obesity. Specifically, a patient with BMI above 25 and under 30 is deemed as over-weight and a patient with a BMI of 35.0 would be considered obese.
This can all be better understood by the ICD-10 codes assigned to each of the BMI ranges.
Some Guidelines:
- Use these BMI related ICD-10 codes when billing obesity counselling services.
- These ICD-10 codes are not only informational but help reimburse these services as their medical necessity.
- Look for medical notes, when not sure about what billable ICD-10 to choose from.
- BMI is usually obtained by clinical staff and documented while taking a patient’s vital signs.
- Even when the terms obese or over-weight is stated (however BMI is not stated), it can easily be assessed from documented weight and the height of the patient.
- Use E66.09 – E66.9 for better explaining other causes of obesity in your claims.
What services can be billed for standard obesity counselling?
G0447 - Face-to-face behavioral counseling for obesity, 15 minutes
G0473 – Face-to-face behavioral counseling for obesity, group (2–10), 30 minutes
HCPCs code G0447 is used for Intensive Behavioral Therapy (IBT) for Obesity or ongoing face-to-face behavioral counseling for patients with a BMI of ≥ 30, who are alert and able to participate in counseling. Medicare and following payers pay for G0447 which can be billed 22 times in a 12-month period counted from the date of the first claim. The valid ICD-10 codes that can be used with G0447 will start from Z68. 30 for BMI exceeding the value of 30. G0447 is a timed code for 15 minutes furnished by a qualified primary care physician or other primary care practitioner in a primary care setting.
Frequency Limitations:
Month 0 - 1:
one visit every week;
Months 2 – 6:
one visit every other week; and
Months 7 – 12:
one visit every month if certain requirements are met
Other reporting specifications:
- At the 6-month visit, a reassessment of obesity and a determination of the amount of weight loss must be documented in the health care record.
- To be eligible for additional face-to-face visits occurring once a month for an additional 6 months, beneficiaries must have lost at least 3kg.
- For beneficiaries who do not achieve a weight loss of at least 3 kg during the first 6 months, a reassessment of their readiness to change and BMI is appropriate after an additional 6-month period.
What services can be billed for Medical Nutritional Therapy (MNT) ?
During MNT sessions a dietitian (or qualified nutrition professional) reviews the changes in the medical condition of the patient, including their diagnosis and treatment regimen. They perform a nutrition screening and review the specific dietary plan for the patient. The provider re-evaluates the diet in such a way that it improves the health and quality of life of the patient.
Following services can be billed for MNT:
CPT 97802 - Medical nutrition therapy; initial assessment and intervention, individual, face-to-face with the patient, each 15 minutes
CPT 97803 - Medical nutrition therapy; re-assessment and intervention, individual, face-to-face with the patient, each 15 minutes
CPT 97804 - Medical nutrition therapy; group (2 or more individual(s)), each 30 minutes
HCPC S9470 - Nutritional counseling, dietitian visit
For Medicare Beneficiaries:
HCPCS G0270 - Medical nutrition therapy; reassessment and subsequent intervention(s) following second referral in same year for change in diagnosis, medical condition or treatment regimen (including additional hours needed for renal disease), individual, face to face with the patient, each 15 minutes
HCPCS G0271 - Medical nutrition therapy, reassessment and subsequent intervention(s) following second referral in same year for change in diagnosis, medical condition, or treatment regimen (including additional hours needed for renal disease), group (2 or more individuals), each 30 minutes
Some Guidelines:
- MNT codes are time-based face-to-face services; the provider must state the total time spent. A minimum of 8 minutes are needed to be spent and documented to report these services.
- These services are provided by Licensed/Registered Dietician or Nutritionist specifically. These services are never billed as ‘incident-to’ services.
- Modifier AE for Registered dietician can be appended to MNT codes. This modifier indicates the services of a nutrition professional or a registered dietician.
- Medical nutrition therapy is limited to three hours of one-on-one contact in the first year.
- Always use the nutritionist’s national provider identifier.
- These services may also be provided via telehealth, which would require the appropriate place of service code and modifier.
- MNT is usually provided after obesity screening (G0447) and the patient is referred to a licensed specialist.
- MNT Codes mentioned below are used in that specific sequence and order starting from initial session.
- Same diagnosis usage rules are applied as stated above along with other illness associated ICD-10 codes.
- These services can be used for eating disorders, obesity, hyperlipidemia, metabolic disorders, Ketogenetic diet, chronic kidney disease (CKD) and other medically necessary conditions.
- Always check with third-party payer policies for reporting these services.
- In some cases, an ABN might be required.
What services can be billed for a ‘healthy’ patient?
If the patient is not necessarily obese or have their BMI under control i.e., the BMI is under <30. First look to E/M or office visits that might include counselling then look into preventive coding for separate counselling sessions that the patient might need for instance 99401-99404 can be used in such cases. These are also time-based codes. The provider will likely counsel the patient on diet, exercise, and obesity and provide behavior change interventions, including assessing readiness and barriers to change, advising a change, or actions and motivational counseling.
AltuMED is a Healthcare Revenue Cycle Management technology and solutions company. Our technologically advanced Practice Management Software, PracticeFit optimizes the Medical Billing workflows for Medical Practices, Labs and Third-Party Medical Billing Companies helping them collect maximum revenue. Find out more
Subscribe to Our Newsletter!
Subscribe to Our Newsletter!
Enter Your Email Address. We Promise We Won't Spam You