
Are you maintaining the Credentialing and Enrollment Status?
A proactive Practice Manager makes sure that the Credentialing and Enrollment process at their Medical Practice is complete. This strengthens patient’s confidence in the patient care services offered.
Now, as the days go by, the daily routine at the Medical Practice gets hectic. Practitioners are consumed with their patients and the staff is busy providing support services as well as taking care of the administrative tasks. The practice manager remains satisfied as all the practitioners are credible and successfully maintaining the patient care status. In all this, there is a high chance that the manager loses the track of time by which the credentialing status of the practitioners is required to be reinstated.
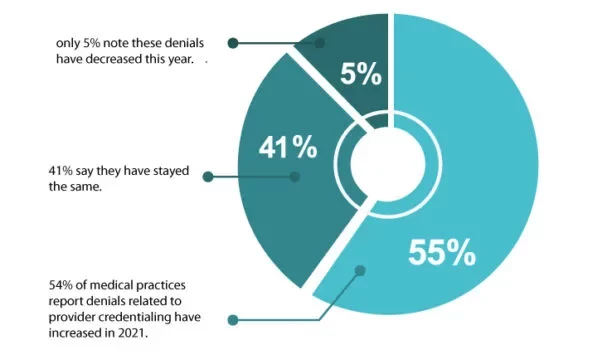
Source: https://www.mgma.com/data/data-stories/more-than-half-of-practices-report-credentialing-r
Problems with an expired Credentialing status
Lost Revenue: If the credentialing status is not updated, the provider is at the risk of deactivation by the payer. This could result in major revenue losses, as the claims for such providers are denied. The re-credentialing process can take up to 180 days or longer therefore proactive planning is crucial.
Loss of Privileges: Expired credentialing can result in loss of hospital privileges. This negatively affects the provider enrollment as providers must have hospital privileges at a participating network hospital in order to join/remain compliant with health plans.
Liability Concerns: Practicing medicine without a valid license/certificate or with an expired one, can open the door to lawsuits for not only the provider, but the provider’s employer/facility as well.
Fines and/or Sanctions: If a provider continues to practice medicine with expired credentials (e.g., writing prescriptions with an expired DEA license), they and their facility may also face significant fines and/or sanctions. Additionally, the provider’s malpractice insurance rates may increase after receiving a sanction.
Refusal of Future Contracts by Payers: Providers who have a history of lawsuits, legal penalties, fines, sanctions, lapsed malpractice insurance, and/or expired CAQH attestation may be rejected by some payers for future contracts.
Low Patient Retention: Providers who do not remain active with payers will fail to attract new patients and risk losing their existing clientele if they become out-of-network and/or must stop providing care until they are re-credentialed.
Additional Work: It takes extra effort and time to reactivate the provider with health plans and obtain hospital privileges again costing the practice valuable resources.
How can expiration of Credentialing and Enrollment status be prevented?
Keeping track of provider credentials is time-consuming and complicated, especially when the provider is taking care of all the tasks themselves.
Hiring a third-party provider with a custom credentialing maintenance and monitoring program can help maintain the credentialing status for the Medical Practice.
A few tips for maintaining the Credentialing and Enrollment Status:

Centralize the Credentialing process

Proactive Monitoring and Planning

A Procedural approach towards Credentialing and Enrollment from the start i.e., when ever a new practitioner is added to the Medical Practice

Proactive Recertification and Recredentialing Status Update
At AltuMED, our credentialing maintenance and monitoring services include:
- A master report for the practice indicating providers with expiring documents at 120, 90, 60, and 30 days out.
- CAQH quarterly attestations (we re-attest the provider every 120 days and upload new documents as they are set to expire).
- Re-credentialing for commercial payers and re-validation for government payers (e.g., Medicare, Medicaid, TriCare).
- Demographic updates, such as address/phone/name change.
- Directory updates; Medicare payers in particular request providers to verify their demographic information every 6 to 12 months.
- Tracking of malpractice insurance coverage, CE credits, and practice services (e.g., Radiology and CLIA certifications).
We also offer a health plan audit service for larger facilities to ensure providers are participating in the correct plans and the provider roster is current. An annual health plan audit is essential for protecting a practice both legally and financially. Contact us to know more about our credentialing and enrollment service.
Practice Credentialing and Enrollment Status Template
Practices face numerous payment issues because of their lack of centralized credentialing and enrollment management. This template provides a strong start for your practice to prevent such issues. The template has two main tabs, the demographics tab compels you to provide your facility’s details, your credentials and contains a credentialing checklist. The payers tab helps you maintain details of the payers, most of the payers for MI area are added but the sheet is editable for your use.
Feel free to contact us for any questions or queries about the attached template or if you want to inquire about the Credentialing and enrollment services.

Subscribe to Our Newsletter!
Subscribe to Our Newsletter!
Enter Your Email Address. We Promise We Won't Spam You
Categories
Informational
Educational
Medical Billing Software
