A Simple Coding Guide for Standardized Assessment, Screening, and Testing for Behavioral Health
The relevance of mental health services in today's busier-than-ever day and age cannot be overstated because they support the CORE fundamentals of our well-being and of those we love. Taking into account, the rocky past and progress in the methods of handling (even the more common) mental and behavioral health conditions. It is wonderful to see how far we have come now that the subject is being talked about and managed in a promising way!
Coming to the main point of this article, May is the month of Mental Health Awareness, taking this opportunity we would like to address how some common mental and behavioral health services can be efficiently billed according to payers’ guidelines about their routine submissions and how to avoid denials impending from a coding perspective.
As more and more related cases are coming forth as the days go by, more advancement in courses of treatment is also being made. We will try to go through them step-by-step and break them down for you, starting from some basic ones.
Let’s start with Initial Evaluations
For the very first interaction with the patient, we have some options to go through. The service you choose entirely depends on several factors at play, which could include:
- Provider’s specialty and credentials (M.D, P.A., NP) OR (a psychologist or psychiatrist)
- Patient’s age (many services are age-dependent)
- Any pre-existing diagnosis or treatment
- Number of screening tests performed before? (Limited units)
- Referrals
Option 1 – E/Ms
This one is obvious for say, any M.D of internal medicine or Nurse practitioner that encounters the patient and feels that they might need to be further evaluated properly for their behavioral health points. So, they might evaluate the patient themselves or make a further referral to a specialist, for which they may bill:
Office Visit: 99202-99215
Inpatient Visit: 99221-99233
(*Or any other related POS- E/M like Home, domiciliary Assisted Living, etc.)
So, these E/M would be somewhere to start.
Remember E/Ms include History and Exam and MDM. The standard formats for E/M can only be billed by practitioners that are allowed under CMS guidelines e.g., Psychologists or Social Workers might not be able to bill E/Ms. The general rule of thumb here is if you can do medication or prescription management you can go ahead and bill those E/Ms.
Option 2 – Standardized Test with Preventive Visits
Annual Depression Screening: G0444
This one is billed once annually with AWVs only as a preventive measure. This is your typical Depression Inventory using a standard test for scoring.
Option 3 – Standardized Screening Tests (Substitute codes)
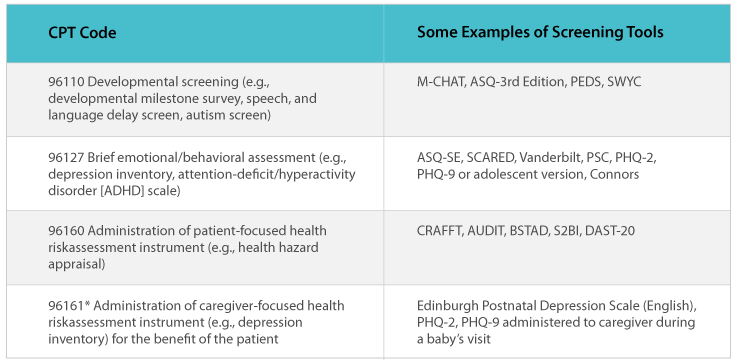
Brief emotional and behavioral assessments performed with standardized instruments: 96127 (GAD-7 or PHQ-9)
This might be the actual next step in the initiation of the course of treatment that might determine the defining diagnosis for the patient. Two ‘Units’ might be billed on the same day with or without the visit for each screening. Diagnosis code Z13.31, “Encounter for screening for depression,” or Z13.39, “Encounter for screening examination for other mental health and behavioral disorders,” usually accompany these claims. A total of 4 units of the services might be billable per year to most payers. If done with AWVs, the diagnosis codes Z00.00 or Z00.01 for normal or abnormal findings respectively will be more applicable.
Option 4 – Standardized Tests (Substitute codes)
Other similar codes that include assessment and intervention for a health risk analysis:
96156 Health behavior assessment, or re-assessment (i.e., health-focused clinical interview, behavioral observations, clinical decision making)
96158 Health behavior intervention, individual, face-to-face; initial 30 minutes
Health and behavioral intervention are the promotion of functional improvements in the patient’s psychological and psychosocial condition. The CPT codes 96156, 96158, 96159, 96164, 96165, 96167, and 96168 may be used only by a Clinical Psychologist (CP). ICD-10 CM diagnosis code(s) reflecting the physical condition(s) being treated must be present on the claim as the primary diagnosis.
96160 Administration of patient-focused health risk assessment instrument (e.g., health hazard appraisal) with scoring and documentation, per standardized instrument
The provider administers a questionnaire aimed at helping to identify a specific health risk to a patient, analyzes the results, assigns a score, and documents the findings. Use this code for each standardized survey questionnaire.
Option 5 – Psychiatric Diagnostic Evaluation
This is where things start to get interesting. As, at this point, we are beyond the standardized tests and tools now. Here, the Provider will perform a full in-length interview with the patient which allows them to better assess diagnosis through integrated biopsychosocial assessment, including history, mental status, and recommendations.
Psychiatric Diagnostic Evaluation – without any medical services: 90791
Psychiatric Diagnostic Evaluation – with medical services: 90792
Medical Services for 90792 might include
Prescription of medication or coordination of medications as part of medical care. Order/review of medical diagnostic studies – Lab, imaging, and other diagnostic studies. Again, the general rule of thumb is followed here which means Psy.D and LCSWs can only be billed 90791 (Evaluation without medical services).
Guidelines on how to bill these codes and avoid denials
- 90792 applies to new patients or patients undergoing re-evaluation. Use this code only once per day regardless of the number of sessions or time that the provider spends with the patient on the same day.
- When the patient goes for a psychiatric diagnostic evaluation, report either 90791 (Psychiatric diagnosis evaluation) or 90792 (Psychiatric diagnostic evaluation with medical services).
- In the past, most payers would allow you to only report one unit of psychiatric diagnostic evaluation code per patient. Now, guidelines have been revised, and payers will allow you to claim for more than one unit of 90791 or 90792 if the initial psychiatric diagnostic evaluations extend beyond one session, as long as the sessions are on different dates.
- An example of this extended evaluation would be when the psychiatrist is evaluating a child and will see the child with parents in one session and then evaluate the child independently in another session. So, depending on medical necessity, you can claim for more than one unit of 90791 or 90792 when the psychiatrist evaluates more than one session spread over more than one day.
- When billing for Medicare, CMS will allow only one claim of 90791 or 90792 in a year. However, in some cases, depending on the medical necessity, Medicare might allow reimbursement for more than one unit of 90791 or 90792. You can also report these codes when the psychiatrist is seeing the patient after a span of three years. Code 90792 has a CCI conflict with code 90791 and with other encounters and psychotherapy codes as well. A modifier is not allowed to override this relationship.
Interactive Complexity (90785) is an add-on code specific for psychiatric services and refers to communication difficulties during the psychiatric procedure. Add-on codes may only be reported in conjunction with other codes, and never alone. Specific communication difficulties are present with patients who typically:
- Have other individuals legally responsible for their care, such as minors or adults with guardians.
- Request others to be involved in their care during the visit, such as adults accompanied by one or more participating family members or interpreter or language translator.
- Require the involvement of other third parties, such as child welfare agencies, parole or probation officers, or schools.
Interactive complexity may be reported with psychiatric procedures when at least one of the following communication difficulties is present
- Requirement to control uncooperative/difficult communication among participants that impairs care delivery (associated, for example, with excessive anxiety, strong reactivity, frequent queries, or disagreement).
- Emotions or actions of the carer that prevent the treatment plan from being carried out.
- Evidence or disclosure of an incident that serves as a sentinel with a requirement to disclose it to a third party (such as abuse or neglect with a report to a state agency) and the beginning of a dialogue with the patient and other visitors about the sentinel event or report.
- The use of playthings, tangible aids, an interpreter, or a translator to get over severe language gaps.
If no psychotherapy treatment is being reported, avoid reporting the CPT add-on code for Interactive Complexity along with psychotherapy for crisis codes or along with E/M services.
Treatment Options – Psychotherapy
All roads (might) lead here! If all the required assessment and screening interventions have been performed accurately and systemically, they will probably lead to Psychotherapy sessions - or famously known as “Talk – therapy”, Most psychotherapy takes place when a licensed mental health professional (Psychotherapist) and a patient meet one-on-one or with other patients in a group setting.
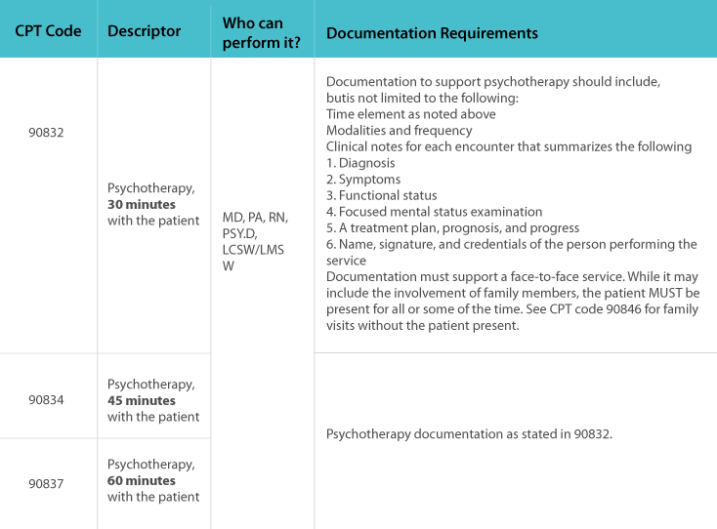
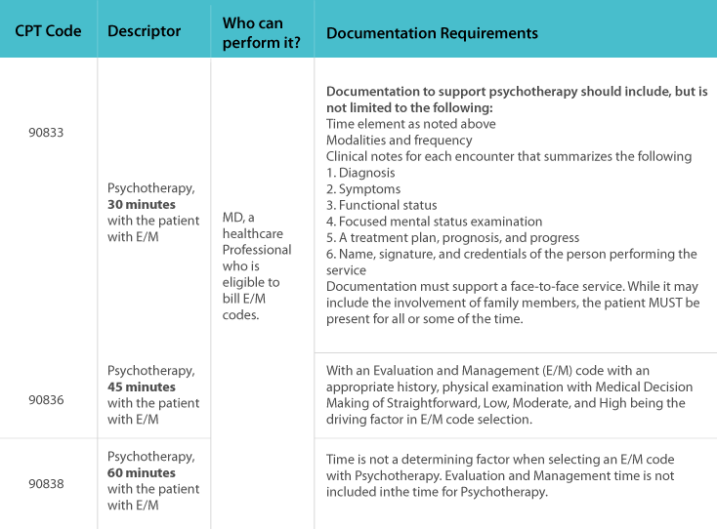
Let’s have a look at standard Psychotherapy codes here
Psychotherapy codes are time-based codes that may be billed with or without the E/M codes
Psychotherapy billed without E/Ms
Psychotherapy billed with E/Ms
Concluding it up….
This whole method of managing behavioral health patients can be better streamlined than how it was used to be the case. Whatsoever the evaluation or screening tools are used, make sure they adhere to the payers requirements and are charged by the established guidelines. Following the process in a step-by-step fashion is a key factor in establishing a differential diagnosis for the patient – which is unique for every patient. This makes it easy for the payers to understand the situation the provider and patients have gone through together to make remarkable progress which inadvertently aids the already stringent process of reimbursing claims for behavioral and mental health claims.
AltuMED Medical Billing Solution is one of the five star rated Medical Billing Companies in Michigan, USA. Contact us for a detailed demo of our Medical Billing Services.
Subscribe to Our Newsletter!
Subscribe to Our Newsletter!
Enter Your Email Address. We Promise We Won't Spam You
Relevant Articles
Categories
Informational
Educational
Medical Billing Software